Some studies estimate that in 25 years’ time, 44% of England’s population will have some sort of condition which will require Long Term Care (LTC). LTC involves those activities that help people who have disabilities and chronic care needs to maintain their levels of functioning and quality of life. These activities are not solely based on health care. Rather, they may entail other actions of daily living such as help with domestic tasks, social inclusion and accommodation for individuals who cannot live independently.
This problem is not only specific to England, though. Instead, the burden of this type of care constitutes a reasonable proportion within the public expenditures of OECD countries. Figure 1 shows that during the last two decades LTC has experienced an increasing growth raising from a 12.5% of the total public expenditure to an almost 16%.
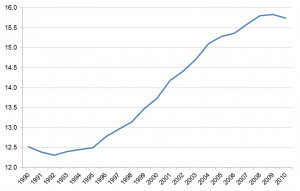 Figure 1: Share of health and long term care spending in total public spending ( in % of total public expenditure) Source: OECD Economic Policy Papers
Figure 1: Share of health and long term care spending in total public spending ( in % of total public expenditure) Source: OECD Economic Policy Papers
Various reasons may explain this rise and the predicted increase in the demand of the LTC during the forthcoming years. Reasons include the demographic move towards an ageing population, low fertility rates, changes in the household’s composition with fewer individuals or higher rates of female participation in the labour market. These may have several economic consequences that policy makers should not disregard when designing the provision and funding schemes which meet both the future demand of LTC services subject to the constraints in suppliers and public budgets.
Firstly, the elements described above may entail changes in the composition of the supply of LTC implying shifts between different types of providers. Given the various types of activities involved, unlike health care, LTC may be delivered by diverse types of providers that include qualified paid carers (formal care) and/or non-paid carers mainly family, friends and charities (informal care). The extent to which formal care can be substituted for informal care entails an important policy debate since informal care is cheaper and in case governments are co-paying part of LTC services, they could have a financial incentive to promote informal over formal LTC. The effects of informal care on formal care have been extensively examined in the empirical literature with generally consistent results. At European level, Bolin et al. (2008) and Bonsang (2009) show that informal care substitutes paid domestic care, although this substitution decreases as the LTC involves more complex clinical needs (e.g. higher disabilities or hospitals visits). UK evidence by Mentzakis et al. (2009) found that there is substitution between informal and formal care for simple tasks but complementarity for cases of complex and technical activities, while Pickard (2012) reports substitution between nursing and care hospitals and the very intense care given by adult children to their older parents.
Likewise, these shifts between providers may imply alterations in other important areas for the economy such as the labour market. Caring is an activity that entails significant opportunity costs. One area where these costs appear more notoriously and which has resulted in a wide empirical literature is the relationships between informal care and labour outcomes. Norton (2000) argues that several topics have occupied the main research interests. These include the associations between the time devoted to caregiving and the wages as well as the effects of informal care on the number of hours worked. Likewise some authors have extended this analysis investigating the influence of carers’ employment status on their willingness to care. Their findings suggested that informal carers would be more willing to care in cases where they bear a low opportunity cost, or in other words, when they don’t have jobs or are relatively low paid. Finally, another area of research has been associated with the relationships between informal care giving and future payments (e.g. inheritances) in order to elicit the supply of caregiving.
A third consequence is referred to the insurance schemes. The majority of research aimed to analyse the impact of formal institutional care on informal care has been focused on studying how different degrees of public insurance affected the intensity of informal care. These studies confirmed certain substitution concluding that more generous public expenditure on formal care (based on financing home care services) are normally associated with lower levels of informal care (e.g Ettner (1994), Stabile et al. (2006) or Viitanen (2007)).
Therefore, the shifts between LTC providers, their effects on other areas of the economy as well as their composition are important issues to consider when thinking about the funding of LTC services from a public perspective. Similarly, bearing in mind the former, policy makers need to explore alternative mechanisms such as the private market for private insurance and understand how demographic and family changes may influence effectively the level of coverage. Van Houtven et al. (2015) address both questions and analysed the opportunity costs in American families showing empirically that factors such as having working spouses or having children living nearby may be likely elements to restrain the purchases of private insurance programs. The design of future LTC plans has demonstrated to be a policy concern for developed economies. As we have seen, a successful strategy will require the coordination of diverse issues.
