By Diarmuid Coughlan
As of July 2015, I started a prestigious Cancer Prevention Fellowship at the National Cancer Institute (NCI) in Bethesda, Maryland USA. Perhaps, the most interesting opportunity afforded to me is to get involved in projects run by the NCI Center for Global Health.
Global Cancer & Research Projects
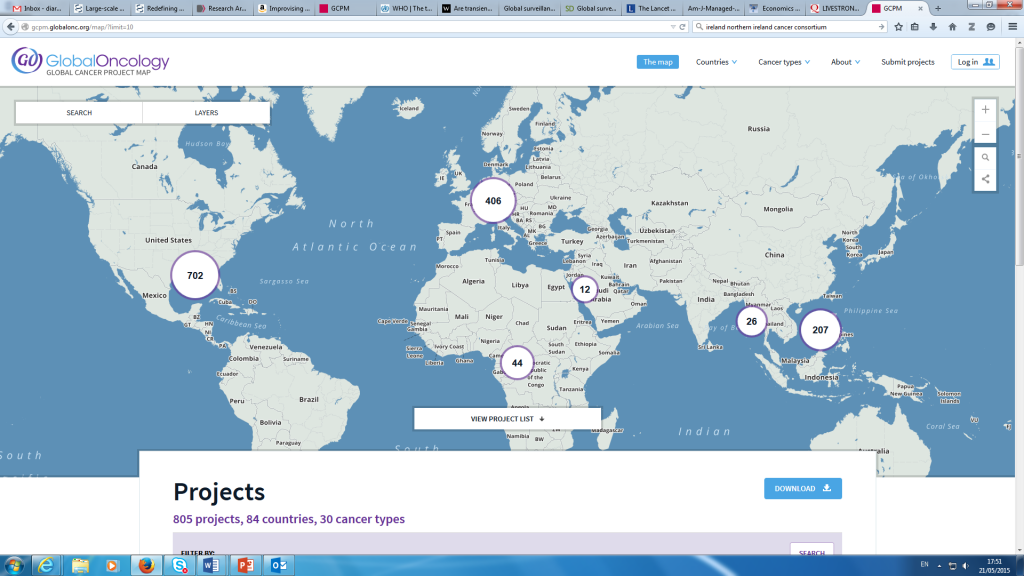
It has been reported by the United Nations that cancer causes more deaths than AIDS, Tuberculosis and malaria in poor countries. Indeed, more than 70% of all cancer deaths occur in low and middle income countries (LMICs). Global cancer epidemiology maps are available from the International Agency for research on Cancer (IARC) and more recently (March 2015) cancer project maps are available from Global Oncology initiative (Based at Stanford) which it is hoped will assist researchers across the globe to collaborate (see Figure 1).
Figure 1: Global Oncology Initiative website facilities international collaboration
In May 2015, at the Ireland-Northern Ireland-NCI Cancer Consortium Conference in Belfast, a lot of international respected speakers spoke about the global burden of cancer and the moral imperative that developed countries have in supporting the cancer research community in LMICs.
Subsequently, at the NCI Summer Curriculum in Cancer Prevention, Dr. Tom Gross gave a stimulating talk about the ‘state of play’ in LMICs and why it’s important that the global community work together as best they can based on some fundamental facts:
Background Facts:
- Cancer is the leading cause of death in the world accounting for 8.2 million deaths or about 15% of all deaths in 2012.
- The global economic cost of cancer was estimated at $1.16 trillion in 2010 (Lopes 2015).
- 25% of cancers in the developing world linked to chronic infection (5% – HPV; 5% hepatitis B and C, 5% helicopter pylori and ~10% arising from various viruses, liver flukes and parasites)
- The rate of cervical cancer incidence [due to human papilloma virus (HPV)] in a country is directly correlated with poverty rates.10-fold more cervical cancer in less developed countries compared to more developed
- Palliative care does not exist in many LMICs
- The single biggest limitation to cancer prevention and policy in LMIC is the lack of a cancer registry to conduct surveillance and population research.
Workforce capacity is another huge problem facing those working in cancer prevention, control and care in LMICs. Many global institutions, academic centres and non-profit agencies are working with partner organisations in LMICs to grow sustainable infrastructure but is a constant challenge to retain qualified medical staff. The emphasis of collaboration has benefits for those in the developed world too – Burkitt Lymphoma is a historical example of how global collaboration can improve patient outcomes globally.
Health Economics
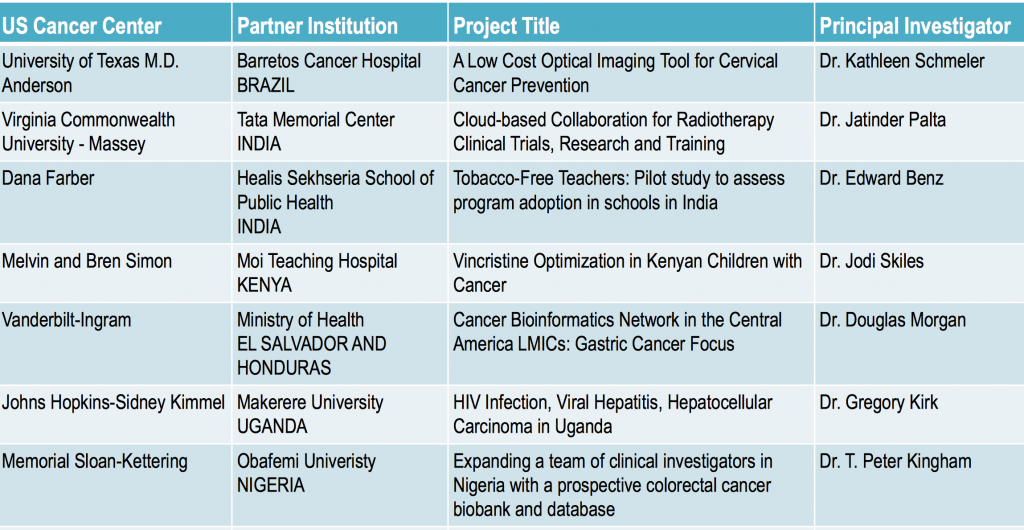
What has become apparent from NCI personnel and Summer Curriculum participants is the importance of health economics in decision-making in LMICs across the cancer continuum. For example, the NCI Non-Communicable Diseases regional infrastructure core planning grants suggests health economics/comparative effectiveness research as one of the seven potential core resources. Furthermore, the NCI supports the development of point-of-care technologies (see Figure 2 for examples) for detection, diagnosis and treatment in LMICs with the following characteristics:
- Portable
- Affordable
- Simple to operate by locally trained staff
- Durable
- Minimally invasive
Figure 2: Examples of NCI-supported grants for LMICs
The most basic construct of whether a technology is cost-effective or not is to use a cost-effectiveness threshold (CETs). Essentially, this is based on the cost per Quality Adjusted Life Year (QALY) metric. This is distinguished from the Disability Adjusted Life Year (DALY), a favoured metric in global health.
The Cost-Effectiveness Threshold in LMICs
In 2014, Paul Revill and Beth Woods (University of York) produced a research paper presenting CETs which are much lower than those previously applied in many countries using WHO recommended CETs of 1-3 times GDP per capita. The York CETs are based on recent empirical estimates of foregone benefit (from the English NHS) and international income elasticities of the value of health. The choice of CET is, therefore, crucial in determining value from healthcare interventions when applying incremental Cost-Effectiveness Analysis.
Final Words
The message from this blog is that the global cancer community are boosting efforts to support cancer research in LMICs. What is encouraging to hear is that health economics/economic evaluation is central to decision-making from supporting research projects to patient treatment and survivorship needs in LMICs.