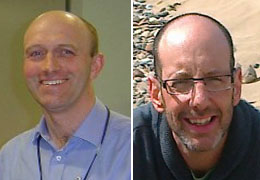
 In the Spring 2016 round of ERDP Development Grants, Drs Steve Jones and Hugh Alberti were funded to carry out a study visit to Harvard medical school to inform the new Newcastle medical school curriculum on longitudinal integrated medical student placements.
In the Spring 2016 round of ERDP Development Grants, Drs Steve Jones and Hugh Alberti were funded to carry out a study visit to Harvard medical school to inform the new Newcastle medical school curriculum on longitudinal integrated medical student placements.
Here is the report of their visit.
Aims
The aim of the visit was to observe first-hand the longitudinal integrated medical student placements (LICs) at Harvard Medical School and in particular to review the practical implications and challenges of implementation. Harvard’s model of “longitudinal integrated clerkship” is a transformative redesign of clinical, largely community-based education involving up to weekly clinics in various specialities. Grounded in the principle of “educational continuity”, students develop a “panel” of longitudinal patients over time in order to observe the patient journey, largely in the community setting but also following patients in and out of hospital. Students also see the patient in the context of their “lived-lives” and develop relationships with them that are grounded in responsibility, commitment and duty. Other key elements of the programme are regular “Bursts” of in-patient duties including on-call time and weekly student-led tutorials. The other key aspect of educational continuity is through a longitudinal relationship with a clinical teacher or “preceptor” in each of the six disciplines. Students join the preceptor in out-patient clinics every week and have a meaningful role in caring for the patients. This would include clerking, presenting and recording in the patient’s notes, following up the patient at subsequent visits and hospital appointments, calling the patient and or visiting them at home.
The Visit
We visited the Cambridge Health Alliance (CHA) over three days: This is associated with Harvard Medical School and is roughly the equivalent of a small base unit in which a group of 12 3rd year students are placed for a LIC for the whole of the academic year. CHA is a cluster of small hospitals with around 150 in-patient beds allied to a number of community “polyclinics.” We were able to observe teaching taking place on the wards, in the polyclinic and a student-led classroom based tutorial. We held discussions with: Preceptors (clinical teachers) from a range of specialties, various faculty staff, students individually and as a larger group, administrators, course directors and both co-founders of the programme and the hospital chief.
Take home messages
Our key take-home messages are; Students have a meaningful, longitudinal role in patient care; Students matter to their preceptors; Students need sufficient white time; Students are responsible for the majority of their learning; The panel of longitudinal cases is key; Admin and IT have an important role to play; Students develop a range of generic and professionalism skills; The hospital reports seeing an increase in the number of residents (junior doctors) applying to work there; Experienced teachers can adapt easily to this model; Specialisation of clinicians may be a challenge but is not insurmountable; An electronic portfolio / log book is essential; Students are better prepared for graduate level learning; Students have the same outcomes / assessments but at different times.
Based on the visit, a number of proposals have been outlined that are being considered by the MBBS Curriculum Review Group. In summary these are an amalgamated LIC model in semester 2 year 4 for all students and a more comprehensive 1 or 2 semester LIC in year 3 for a smaller number of students.
Steve Jones and Hugh Alberti, October 2016
