Registration is open for our annual European Cardiovascular Development and Regerneation meeting. After the wonderful sucess of our Paris 23 meeting, we now go to Prague and are hosted by Professor David Sedmera. Some of you will remember when we were in Prague some years ago – that was a pretty fantastic event!
This year we are having a meeting sponsored and endorsed by the European Society of Cardiology, but organised by Charles University. This has simplified the organisation and also kept the cost down.
Meeting website: https://icdar.lf1.cuni.cz/index.html
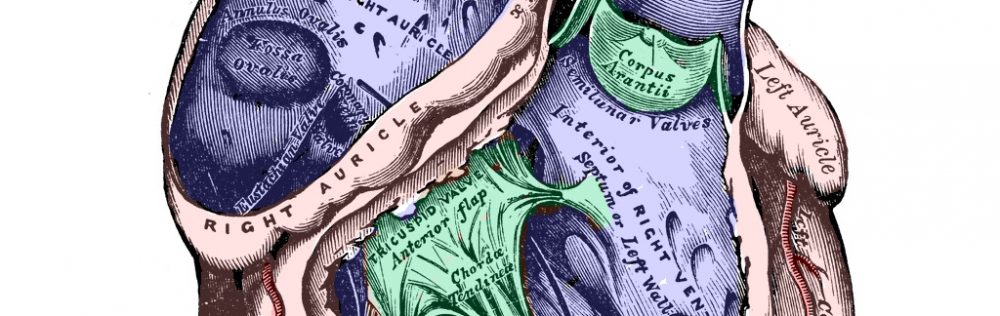
Can I suggest you register for the meeting as soon as possible. There are limited places at the Hands-on anatomy session and we also have a last night gala dinner.
The Key Note speakers will be Professor Richard Harvey from Australia and Maurice van den Hoff from Amsterdam.
We will have our usual format of sessions – dictated by the abstracts we recieve from the delegates (so send them in). As expected we will keep the quese for coffee short and the poster sessions (with beer) long. There will be an important AGM – we have lots of news to tell you
Any questions – just email me – bill.chaudhry@ncl.ac.uk and I can sort you our or direct you to the right place.
There are loads of hotesl to choose from – David has a couple of selections on the website (I’ll be at the Novotel Praha Wenceslas Square
See you at the Weinstein or see you in Prague or see you at both!