By Professor Robert Lightowlers
In 1988, scientists in the UK and US recognised that certain diseases were caused by mutations in mtDNA . Over the following 20 years, mtDNA defects have been shown to cause a range of debilitating diseases many affecting different parts of the body. However, the main disorders relate to your muscle tissue and the brain.

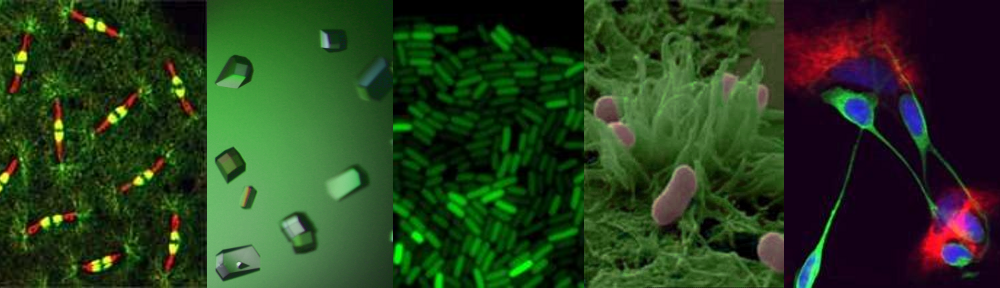
Human muscle fibres stained for mitochondrial function. As can be seen in B, some of the fibres show no activity. This is because these fibres have high levels of mutated mitochondrial DNA.
It is estimated that at least 1:10,000 people suffer from disorders associated with defects in Mitochondrial DNA (mtDNA) – that’s more than 6,000 people in the UK. Even so, it is only recently that the importance of mitochondrial diseases have hit the general media.
Many of you will have seen the debate on correcting mitochondrial diseases in the newspapers (for example, see the Guardian, Telegraph) and on television recently, but not be aware of the central role that Newcastle researchers have played in making this exciting, or to some, controversial, new therapy closer to becoming a reality. Here, Bob Lightowlers ICAMB Director and senior member of the Wellcome Trust Centre for Mitochondrial Research (WTCMR) reflects on the role mitochondrial research in Newcastle has played in this process over the last 20 years and tells us some of the story behind the headlines.
What are Mitochondria?

Electron micrograph of a cell (coloured blue) revealing part of the mitochondrial structure (orange) within. The entire length of the mitochondrion is about 5 micrometres.
These crucial structures found in all the trillions of cells in our body have many essential functions. One very important role they play is to take our common foodstuffs such as fats and sugars and turn them into energy for our body’s to function.

A single human cell showing the nucleus (green), the mitochondrial network (red) and the mitochondrial DNA within the network (yellow)
One surprising element of these structures is that they contain their own genetic element, mitochondrial (mt) DNA. Much smaller than our chromosomes, mtDNA is essential for energy production.
OK, so this is important, but why have mitochondria and mtDNA begun to work their way into the common conversation of the nation?
Answer: Our mothers!
What has this got to do with our mothers ? Mitochondrial DNA is only transmitted to babies by their mothers. This is different to all our other DNA where copies are made and transmitted from both parents. Unfortunately, as you inherit your mothers mitochondria, diseases caused by mtDNA mutations are inadvertently transmitted from the mother.
How does this relate to Newcastle based Mitochondrial Research?
My colleague Doug Turnbull, a neurologist here in Newcastle (and Director of the WTCMR) and I have been intrigued by these mtDNA mutations since it first became clear that they could cause disease. Back in the early ‘90’s, we discussed whether some day it would be possible to try and prevent the transmission of the faulty mtDNA from the mothers to their children. Of course, at that stage, it was just wishful thinking. As the Mitochondrial Research Group (MRG) began to grow and mature in Newcastle, we often returned to one question:
What if the nucleus from the diseased egg could be transferred to a healthy egg whose nucleus had been removed, in essence leaving all the affected mtDNA behind ?
If it was indeed possible, this reconstituted egg could be fertilised and implanted back into the mother by standard techniques used routinely in fertility clinics throughout the world. We also would consider when would such a technique be most efficient: before or after fertilisation of the egg? On paper both options looked possible, but there are many complications.
Technical Concept: achieving the switch of nuclei without some of the faulty mtDNA being inadvertently taken along for the ride.
Towards the end of the 90’s, scientists working in Canada were able to show that the level of mtDNA inadvertently transferred when the nucleus was switched into a recipient cell lacking a nucleus, was low. This was a promising result, but it led to two central questions:
• Could this be repeated with human cells?
• Was this technique morally and ethically acceptable to everyone?
The ethical debate: Debate raged as to whether this technique would constitute genetic manipulation of humans, which of course would be illegal. Further, it was not possible to perform these types of reconstruction experiments in man, as using viable human fertilised cells for research was also, understandably, illegal.
Professor Mary Herbert working at the nearby Human Fertility Centre came up with an intriguing proposal. She explained that unfortunately, during the standard process of in vitro fertilisation, many eggs became incorrectly fertilised. These eggs are unable to grow correctly and have to be discarded. One way of determining whether it would be possible to swap mtDNA in humans, she suggested, was to use these incorrectly fertilised eggs. As this procedure would still require the manipulation of fertilised human eggs, a licence would need to be applied for from the Human Fertilisation and Embryological Authority (HFEA). Following lengthy and extensive debate, including members of the research team being called to the House of Commons, a licence was eventually awarded in 2005. Five years later, with the essential help of colleagues in the Fertility Centre, Mary, Doug and a group of us from the MRG were able to show that such a swap could be performed without any or very low levels of the defective mtDNA being transferred. Importantly, there was also no defect detectable in the reconstituted cells . In 2011, this very promising result, along with many other important contributions made by the Newcastle MRG to understanding mitochondrial biology in health and disease was recognised by the Wellcome Trust who funded the establishment of a new Research Centre in Newcastle, the Wellcome Trust Centre for Mitochondrial Research.
Getting acceptance of the technique
It was important to know whether the people of the UK agreed that such reconstitution technology was ethically acceptable. In August 2012, the government asked the Human Fertility and Embryological Authority (HFEA) to find out what the general public thought of the procedure . The results were collated last month and the Human Fertility and Embryological Authority made a recommendation to Government. There was an overall support for the new technology with only 10% being fairly or strongly against the concept of mitochondrial gene replacement ) This is an endorsement of the method but there is still a long way to go before the technique can be performed in the clinic.
Its amazing to think how far this concept has come in 20 years. Perhaps in another 20 years we may be able to look back and celebrate how this dream has helped to provide a realistic method to help prevent the transmission of a debilitating disease for many couples.
Wellcome Trust Centre for Mitochondrial Research http://www.newcastle-mitochondria.com/
Human Fertility and Embryological Authority (HFEA) http://www.hfea.gov.uk/index.html
HFEA mitochondria puclib consultation 2012 http://www.hfea.gov.uk/6896.html