With obesity rates at crisis point across the UK, Dr Tim Townshend, Director of Planning and Urban Design within the School of Architecture, Planning and Landscape, discusses the part that our built environment has to play. Part of the Newcastle University Institute for Social Renewal‘s Ideas for an Incoming Government series, Dr Townshend argues that central government and local authorities need to take action now to promote healthy living in our communities.
What is the problem?
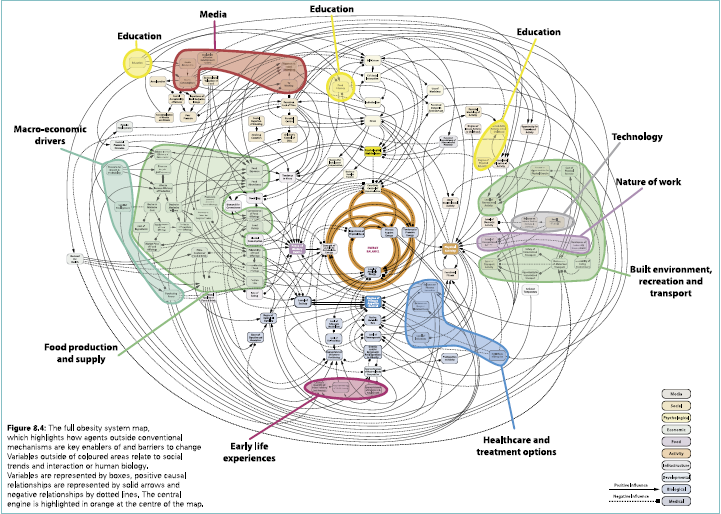
Rates of obesity have reached crisis point, with accompanying health problems (type 2 diabetes, coronary heart disease etc.). In 2007 the Foresight Report ‘Tackling Obesities: Future Choices’ suggested there was enough expert evidence to implicate built environment in the obesity crisis. The places where we live, work, go to school and spend our leisure time can either provide, or constrain, opportunities for physical activity and access to both healthy and unhealthy food. However, the planning system in England is ill equipped to act on this evidence.
This needs action now. Even if the influence of the built environment is small at the individual level, given its impact is over whole communities and that it generally survives several generations unchanged, it is highly significant in aggregate. The change in policy initially needs to address the National Planning Policy Framework (NPPF). The NPPF calls for the planning system to promote ‘healthy communities’, but it is vague in its focus and how this might be achieved.
Obesity is not the only health crisis to face the country – however, it is one in which intervention in the built environment could make a significant difference and interventions to tackle obesity have the potential to deliver broader health and well-being benefits. For example, there is evidence that providing adequate good quality open spaces will encourage physical activity – we also know that physical activity and greenery/green space are also linked to improved mental health and well-being. Moreover obesity is also a problem that has a distinct socioeconomic profile – poorer communities are more adversely affected by obesity and related health/well-being issues than their better off neighbours – and therefore addressing this issue can help tackle health inequalities through the planning system.
The Solution
Action by Central Government/ Department of Communities and Local Government (DCLG)
The NPPF:
- The NPPF (or its replacement) needs to be strengthened – it should state that planning policies must deliver (not merely promote) environments that support healthy lifestyle choices.
- The NPPF should be clear that policies that deliver healthier environments should be enshrined in core polices of the Local Development Framework (LDF) – i.e. not just Supplementary Planning Documents (SPD) so they carry enough weight to be acted upon.
- The viability clause – paragraph 173 – must be rewritten. The elements which support healthy lifestyles, good quality public realm, greenspace, bespoke cycle provision are expensive – however ‘viability’ should not be used as an acceptable reason to remove elements of design in the planning process which are proven to be linked to healthy behaviours and outcomes.
More broadly non-planning actions DCLG should consider include:
- Including directives that aim to improve health and wellbeing in other built environment guidelines – such as UK Building Regulations
- Introducing a ‘healthy lifestyle’ kitemark or rating system (like that used for energy efficiency) for new buildings, particularly housing.
Action by Local Authorities
Local authorities should have planning policies that:
- Deliver healthier lifestyles and greater well-being through the built environment incorporated in their Local Development Framework – to ensure enough weight is attached to these policies. Supplementary Planning Documents may be used to support and/or enhance core policies.
- Enable ‘active travel’ (walking/cycling) to be ‘designed in’ as part of everyday life for communities wherever possible
- Ensure adequate greenspace – in its full variety of forms (pocket parks; parks; sports pitches; garden allotments; wildlife areas etc) – is provided, particularly when new housing is developed
- Restrict the proliferation of fast food outlets – in particular prohibit new outlets in the proximity of schools and children’s centres
More broadly:
- Ensure the new public health responsibilities in local authorities (Public Health Boards etc.) are fully linked into to planning practice – for example through robust review processes.
The evidence
There is a vast body of evidence, it’s not all in a form that can be used by planning – however the Government Office for Science Foresight Report provides a useful summary:
FORESIGHT 2007. Tackling Obesities: Future Choices – Project report. London: Government Office for Science.
Also see:
LAKE, A. & TOWNSHEND, T. 2006. Obesogenic environments: exploring the built and food environments. The Journal of the Royal Society for the Promotion of Health, 126, 262-267.
TOWNSHEND, T. G. & LAKE, A. A. 2009. Exploring obesogenic urban form, Theory, policy and practice, Health and Place, 15, 909-916.
Townshend T.G. (2014) Walkable Neighbourhoods: principles, measures and health impacts, in Burton E., & Cooper, R Well-being and the Environment, Oxford, Wiley-Blackwell
TOWNSHEND, T.G., GALLO, R. & LAKE, A.A. (May 2015) Obesogenic Built Environment: Concepts and Complexities in BARTON, H., GRANT, M., THOMPSON, S., & BURGESS, S. (Eds) The Routledge Handbook of Planning for Health and Well-being, Abingdon, Routledge.